A new study has come out on reference pricing by the California Public Employees’ Retirement System (CalPERS). To be specific, it's about what I call horizontal reference pricing. In this style of reference pricing, one price is set for a procedure or episode of care for a specific condition and applied across facilities. The consumer is on the hook for any amount charged above the reference price. (This post contrasts this with vertical reference pricing—such as that used for prescription drugs in many European countries.)
Reference pricing is currently permitted for large-group and self-insured plans by the Department of Health and Human Services provided the price is set so that consumers have sufficient access to care, it is only applied to services for which consumers have time to shop for care, and that safeguards are in place for patients with additional limitations (e.g., more comorbidities or additional geographic constraints on access).
James Robinson and colleagues studied CalPERS' shift to reference pricing for colonoscopy in its PPO product. Colonoscopy prices, like those of many procedures, vary tremendously across providers. And, as documented by Kathleen Carey, for many procedures—including colonoscopies—offered at both ambulatory surgical centers (ACSs) and hospital outpatient departments (HOPDs), hospitals' prices are higher and have grown more rapidly.
The new CalPERS payment policy was designed in response to much higher HOPD prices for colonoscopies relative to ACS prices. Under the policy, the latter were paid their usual, negotiated price and the former's price was capped at $1500, the reference price. As in prior analysis of CalPERS' reference pricing by Robinson and colleagues, Anthem Blue Cross served as a comparator.
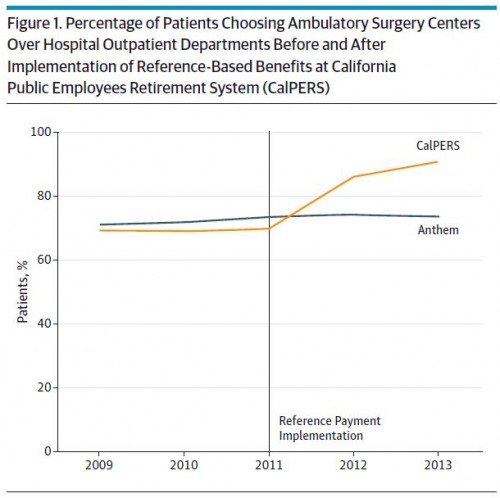
The following two figures tell most of the story. Figure 1, just below, shows a large increase in the percentage of CalPERS patents choosing ASCs for colonoscopy after the reference pricing policy went into effect, relative to Anthem (whose percentage stayed flat).
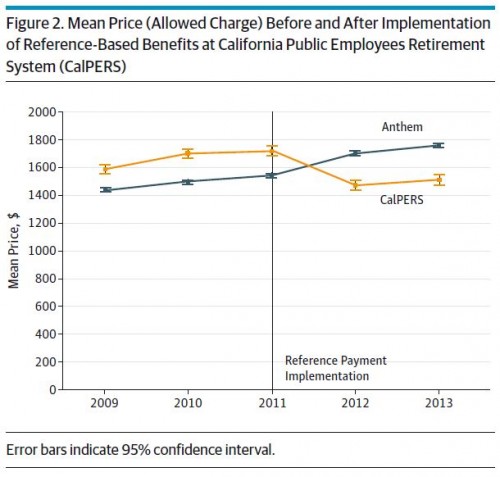
Consequently, and not surprisingly, Figure 2 shows that average price of colonoscopies fell for CalPERS. Anthem's rose.
The investigators found no statistically significant changes in rates of complications, so the change in site of care did not come at the expense of measured quality. However, in an accompanying commentary, David Lieberman and John Allen pointed out that the study did not measure adenoma detection rate and other aspects of quality. (They wrote that adenoma detection rate "has been linked to the development of interval cancers after colonoscopy.")
Over two years, CalPERS' reference pricing of colonoscopy was associated with a $7 million saving (or 28%). This study is the latest in a series of papers on CalPERS reference pricing for a variety of procedures. I've written them and related topics on this blog. Here's a sample of posts:
- "Reference pricing as an alternative to selective contracting" (AcademyHealth blog, 12 September 2013) considers CalPERS reference pricing for knee and hip replacement surgery. According to work by James Robinson and Timothy Brown, it was associated with a $7,000 reduction in price per procedure and saved CalPERS $3 million in 2011.
- "Reference pricing, what could possibly go wrong?" (AcademyHealth blog, 27 January 2015) discusses some of the limitations of reference pricing. It's only feasible for elective services and in a market with sufficient provider competition and with price and quality transparency, perhaps limiting it to 5% of health care spending, according to one estimate. (See also the critique of reference pricing by David Frankford and Sarah Rosenbaum, and their recommendations to federal agencies.)
- "The latest on reference pricing" (AcademyHealth blog, 9 June 2015): Summarizes the work of by James Robinson, Timothy Brown, and Christopher Whaley, who examined the reference pricing by CalPERS for cataract removal surgery. Reference pricing was associated with a payment reduction of 19.7%, saving CalPERS $1.3 million over two years.
At least in terms of spending, CalPERS appears to be enjoying tremendous success with reference pricing. Will other insurers and programs follow its lead?
Austin B. Frakt, PhD, is a health economist with the Department of Veterans Affairs, an Associate Professor at Boston University’s School of Medicine and School of Public Health, and a Visiting Associate Professor with the Department of Health Policy and Management at the Harvard T.H. Chan School of Public Health. He blogs about health economics and policy at The Incidental Economist and tweets at @afrakt. The views expressed in this post are that of the author and do not necessarily reflect the position of the Department of Veterans Affairs, Boston University, or Harvard University.