Has the digitization of health records hurt the practice of medicine? This is a major question hanging over one of the year’s biggest health tech conferences, Health Datapalooza. Electronic health records (EHRs) have come under fire in recent months — for being a source of daily frustration, distraction, and errors. These complaints, however justified, bring to light the need for the medical community to create something better. Doing so will require two big changes: first, software companies need to make their platforms more flexible, and, second, medical teams to take more ownership over the design of the software used within their practices.
How a “pain point” for physicians ends up hurting patients
Last week, Kaiser Health News and Fortune published a deep dive into “where EHRs went wrong,” revealing how flawed corporate and public policies combined with faulty software design to inject a range of problems into health care—from routine annoyances to tragic consequences. No one has been more vocal in criticizing EHRs than doctors themselves. Atul Gawande wrote last November: “We’ve reached a point where people in the medical profession actively, viscerally, volubly hate their computers”
Dr. Gawande is not alone. The Physician’s Foundation’s 2018 Survey of American Physicians cited excessive time spent in front of a computer as the leading source of physician burnout — both during patient visits and after hours. In some specialties, physicians spend nearly half their time looking at a screen during a shift plus additional time entering data into EHRs every day afterhours. I remember when physicians used to spend our afterhours reading up on the latest medical literature and spent our shift hours getting to know our patients; an impossible task now with the rapid changes in medicine.
Of course, physician burnout hurts the profession, but it has much wider implications for patient health. By 2025, the U.S. Department of Health and Human Services predicts that there will be a nationwide shortage of nearly 90,000 physicians, many driven out of the field due to the effects of burnout. A January report from Harvard, the Massachusetts Medical Society, and the Massachusetts Health and Hospital Association declared physician burnout a “public health crisis” requiring “significant changes to the usability of EHRs.”
We need digital health records that reflect the on-the-ground realities of medicine
Medicine is a fast-changing discipline, and some specialties (like cancer) change even faster than others. EHRs originally promised to make our profession more efficient. But in my experience, most out-of-the-box software proves too slow and clunky to keep up. Commercial EHRs also have a major blind spot: they do not reflect up-to-date treatment pathways. This is problematic in many cases — the most obvious of which is when the FDA approves a new drug. If you or a loved one were sick, wouldn’t you want your physician to know about every treatment option available?
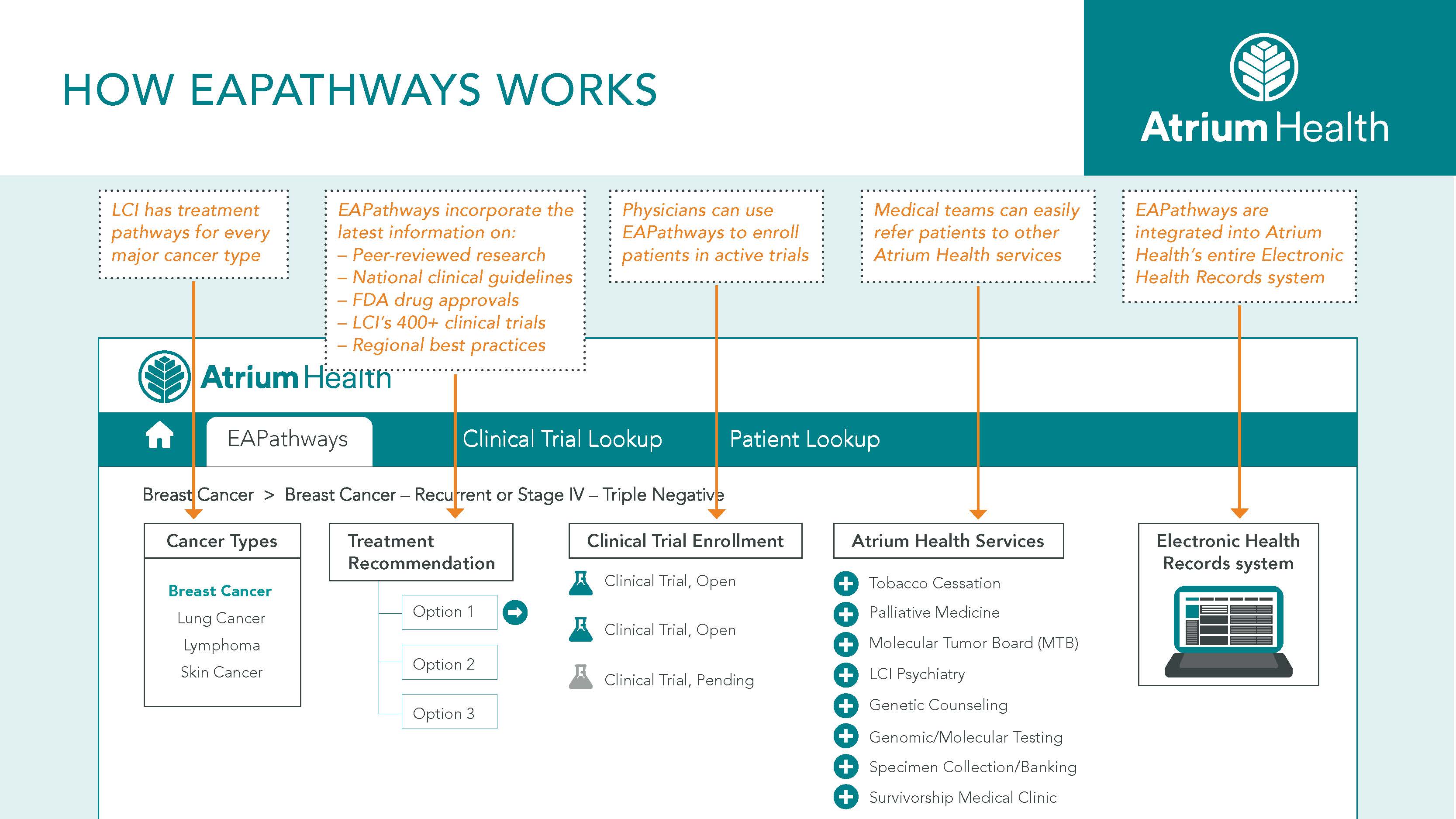
Given the shortcomings of commercially available EHRs, four years ago, physicians at Levine Cancer Institute came together to design our own digital platform, built on top of the EHR used by our entire health system. This non-commercial platform, called Electronically Accessible Pathways (EAPathways), distills the latest clinical guidelines, scientific literature, drug approvals, and physician best practices into a single step-by-step process. EAPathways can be centrally accessed by physicians, nurses, and pharmacists across our 25+ sites and updated in real-time. The platform has been embraced by our medical teams because of its ease of use and improved daily care across a large regional-based system. A physician-built platform like ours proves how the same people who use EHRs on a daily basis could design and revive them.
The future should be flexible
Despite how profoundly EHRs have changed the day-to-day practice of medicine, most medical teams today have little say in their design. Only a small fraction of EHRs today are “self-developed” by hospitals or care providers.
At #hdpalooza, I’m sitting down with Friends of Cancer Research, the American Society of Clinical Oncology, and the National Cancer Institute to discuss how physician-built IT systems and software can transform the practice of medicine.
Much discussion around the future of EHRs has emphasized “interoperability”— which would allow providers to easily share records anywhere in the country. While I agree wholeheartedly in the importance of more easily sharing medical records across facilities, medical tech providers and federal regulators should also focus on the need to make software customizable by frontline specialists and local practices. We as medical experts know our patients and work environments better than anyone else does. But we need more control over existing EHR software in order to heal its many ailments.
The opinions expressed in this blog post are the author's own and do not necessarily reflect the view of AcademyHealth.