I've known for some time that many commercial market health plans have adopted Medicare's hospital payment system, which is based on diagnosis-related groups. What I did not know was whether the health systems of other nations have done so as well. A recent Health Affairs paper by Wilm Quentin and colleagues explains that some have followed Medicare's lead. In particular the authors examine the systems of England, France, Germany, the Netherlands, and Sweden.
European countries often look to the United States for inspiration and innovation in ways of organizing and paying for health care. [...] In England, France, Germany, the Netherlands, and Sweden DRG-based hospital payment systems were introduced between 1995 and 2005—one or two decades after the introduction of the Medicare inpatient prospective payment system.The first sentence of the quote above is also the first sentence of the paper. It took me a moment to get past it. It's a bit stunning that European countries that spend far less than the U.S. and achieve generally comparable or better outcomes would want to emulate anything from our system. And yet, they do. That they do emulate Medicare, at least in one respect, and achieve more efficient results suggests that not everything about Medicare is to blame for the shortcomings of the U.S. system. Yet, there are some differences between European DRG-based payment systems and ours. From them, the authors suggest the U.S. might learn a thing or two. The chart below, which I made from data in the paper, illustrates just two of the many differences.
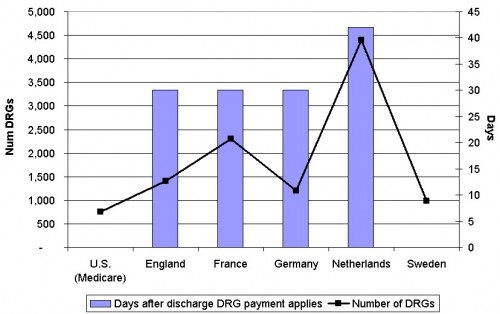 First, the U.S. uses the fewest number of DRGs (black line, left-hand scale). A larger number permits more refined adjustment of payments for disease type and severity. The authors suggest this may make it more difficult for European hospitals to specialize in profitable patients than in the U.S. I'm not sure I've ever heard a call for more payment complexity in the U.S., but this is evidence consistent with the notion that it may have benefits.
Second, the number of days after discharge for which the DRG payment applies is lowest in the U.S., though tied with Sweden: zero (blue bars, right-hand scale). Other systems have more of an episode- than discharge-based model, bundling the care received for 30 or more days after discharge.* DRG payments in all but the Medicare system apply to physicians, not just hospitals, so payment is really for a broader, not just longer, bundle of care.
Moving toward bundled, more episodic payments is a goal embodied in the Affordable Care Act, but combining Medicare payments for physicians and hospitals is not. The bifurcated payment system perpetuates documented obstacles to aligning incentives for efficient delivery of care (PDF).
Perhaps it is time we learned a few lessons from Europe.
* There are some exceptions to the number of days reported for some of the European systems, as indicated in the paper.
First, the U.S. uses the fewest number of DRGs (black line, left-hand scale). A larger number permits more refined adjustment of payments for disease type and severity. The authors suggest this may make it more difficult for European hospitals to specialize in profitable patients than in the U.S. I'm not sure I've ever heard a call for more payment complexity in the U.S., but this is evidence consistent with the notion that it may have benefits.
Second, the number of days after discharge for which the DRG payment applies is lowest in the U.S., though tied with Sweden: zero (blue bars, right-hand scale). Other systems have more of an episode- than discharge-based model, bundling the care received for 30 or more days after discharge.* DRG payments in all but the Medicare system apply to physicians, not just hospitals, so payment is really for a broader, not just longer, bundle of care.
Moving toward bundled, more episodic payments is a goal embodied in the Affordable Care Act, but combining Medicare payments for physicians and hospitals is not. The bifurcated payment system perpetuates documented obstacles to aligning incentives for efficient delivery of care (PDF).
Perhaps it is time we learned a few lessons from Europe.
* There are some exceptions to the number of days reported for some of the European systems, as indicated in the paper.