I've written about telemedicine on this blog and at The Upshot, but neither post covered some recent work that nicely characterizes its state and hints at its future.
In an issue brief for the Health Care Cost Institute (HCCI), Fernando Wilson and colleagues report the number of state laws pertaining to telemedicine. The growth in state legislative activity pertaining to telemedicine is conveyed in their chart reproduced just below. Half of all such laws were enacted in the last five years.
[caption id="attachment_70084" align="aligncenter" width="500"]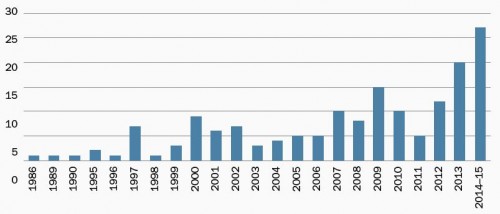 Number of state telemedicine laws by year of implementation[/caption]
Number of state telemedicine laws by year of implementation[/caption]
Naturally, not every state regulates telemedicine the same way. One way to categorize state regulations is according to the three main types of telemedicine:
- Live video — This is what it sounds like, the use of video transmissions to allow patients and providers to interact, remotely and in real time
- Store and forward — The capture of images (e.g., radiologic or of skin conditions) or signals (e.g., electrocardiogram) for future examination by a remote specialist
- Remote patient monitoring (RPM) — Real time conveyance of patient vitals and conditions (e.g., those for a patient in an ICU) to distant providers
The chart below, from the same HCCI issue brief, indicates which states have enacted policies pertaining to each type of telemedicine. Twenty-four states have laws pertaining to live video. Among them, 21 require insurers to reimburse for service so delivered. Fourteen states have enacted store and forward policies, four of which require coverage for it. Six states have RPM policies, four requiring coverage.
[caption id="attachment_70085" align="aligncenter" width="500"] Number of states with enacted telemedicine policies, by transmission mode (RPM = remote patient monitoring)[/caption]
Number of states with enacted telemedicine policies, by transmission mode (RPM = remote patient monitoring)[/caption]
A natural question is, to what extent are telemedicine services being delivered and how have they grown? Using data from five large insurers covering over 50 million people and spanning care delivered between 2009 and 2013, Wilson et al. examined telemedicine use by primary care physicians. It'd be an overstatement to say it's modest. Of nearly 100 million primary care claims over that period, only about 6,500 were for telemedicine services (about 0.0065%).
[caption id="attachment_70095" align="aligncenter" width="500"] Number of primary care telemedicine claims (2009-2013). * denotes fewer than 10.[/caption]
Number of primary care telemedicine claims (2009-2013). * denotes fewer than 10.[/caption]
And yet, telemedicine use has nearly doubled from 2009 to 2013. It quadrupled since 2010. (For some reason it halved from 2009 to 2010. I don't know why, and neither do the authors, but it's one reason to be a little suspicious of the data, at least for 2009.)
Telemedicine is not reimbursed to the same extent as in-person visits. In 2013, the average reimbursement for a regular visit was $68. For telemedicine it is $38, or 45% lower. Perhaps it's the lower reimbursement rate that explains low use of telemedicine services, though one might expect the cost of telemedicine to also be somewhat lower.
However, things could change, at least in some states. As of last year, seven states (Arkansas, Delaware, Hawaii, Minnesota, Mississippi, Tennessee, and Virginia) require commercial market reimbursements for telemedicine be on par with in-person visits. Wilson et al. also offer that it's possible there's some delay in physician practice response to the changing telemedicine environment.
In interpreting rate of change in telemedicine use, we also cannot rule out data issues. "One [14-year old] study of teleconferencing use in a university hospital found nearly one-third of teleconferences were not logged and thus not billed," the investigators wrote. And, it needs to be emphasized that the Wilson study is only of primary care claims and only from five insurers. Other physicians reimbursed by other insurers, as well as public programs, may use telemedicine to a larger extent.
I think it's likely telemedicine will continue to grow, even accelerate. One quarter of patients in the US do not have or lack access to a primary care provider and telemedicine is one way to improve access. In various ways, the Medicare program and the Affordable Care Act increasingly support telemedicine. According to a study by Jennifer Polinski and colleagues, the vast majority of patients are satisfied with telemedicine.*
We are several decades into the information age. Consumers are accustomed to information services — as much, though not all, of medicine is — to be available electronically, on demand (or at least with far less waiting), and far more conveniently than doctor visits have historically been. Though regulations and low payment rates may slow telemedicine, I don't think they will stop it. I think, in time, they will change to meet demand.
* It should be noted that this finding is based on a survey of patients that self-selected into telemedicine and without contrast to comparable patients experiencing in-person visits.